
When a person or a loved one receives a diagnosis of a serious, life-limiting illness, the world can feel like it’s spinning out of control. In the midst of clinical jargon and complex treatment plans, it is easy to lose sight of the person behind the patient. This is exactly where palliative care steps in. Far from being a “last resort,” this specialized medical field is designed to wrap a layer of support around patients and their families, focusing on quality of life, comfort, and emotional well-being from the moment of diagnosis.
A Clear Explanation of Palliative Care
Essentially, palliative care acts as an additional layer of professional medical support specifically tailored for those living with the daily stress of a severe illness. This specialized approach prioritizes alleviating the physical discomfort and psychological strain associated with serious health conditions. At its heart, this care aims to elevate the well-being of the patient while simultaneously supporting the entire family unit.
Unlike hospice, which is specifically for the end of life, palliative care is accessible from the moment of diagnosis, functioning as a supportive layer of care that runs parallel to your curative medical treatments. Think of it as a parallel track: while your primary doctors work on treating the disease, the palliative team works on treating the person.
The Multidisciplinary Team
Palliative care isn’t just about a single doctor. It involves a coordinated team approach designed to cover every aspect of a patient’s needs. Organizations like Iris Medical Group specialize in bringing these diverse professionals together to ensure care is seamless. This team typically includes:
-
Palliative doctors and nurses.
-
Social workers.
-
Nutritionists and pharmacists.
-
Chaplains or spiritual counselors.
-
Massage therapists or music therapists.
How Palliative Care Is Different From Hospice
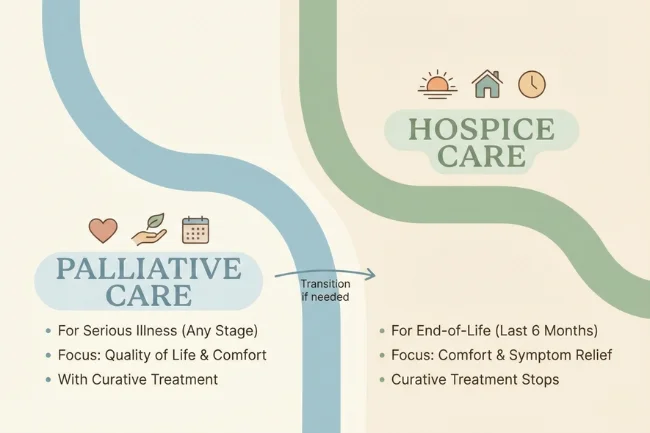
One of the most common misconceptions is that choosing palliative care means “giving up.” This assumption is entirely incorrect. While both focus on comfort, their timing and intent differ significantly.
Comparing the Two Paths
Who Can Benefit from Palliative Support?
Palliative care is appropriate for individuals of any age and at any stage in a serious illness. It is commonly utilized for chronic and progressive conditions such as:
-
Cancer (at any stage).
-
Congestive Heart Failure (CHF).
-
Chronic Obstructive Pulmonary Disease (COPD).
-
Kidney disease.
-
Alzheimer’s and other forms of dementia.
-
Neurological disorders like ALS or Parkinson’s.
Managing the Burden of Symptoms
Living with a serious illness often involves more than just the primary disease; it involves a cascade of side effects. The palliative team specializes in managing:
-
Pain: Utilizing a variety of medications and therapies to ensure physical comfort.
-
Respiratory Issues: Helping patients manage shortness of breath or “air hunger.”
-
Digestive Distress: Addressing nausea, constipation, or loss of appetite.
-
Fatigue: Finding ways to preserve energy for what matters most.
The Pillars of the Palliative Approach

To understand how this care works in practice, we have to look at the three main pillars: Relief from symptoms, emotional reassurance, and care planning support.
1. Physical Symptom Management
The most immediate benefit is the reduction of physical suffering. According to the Center to Advance Palliative Care (CAPC), early intervention in palliative services can lead to better adherence to treatment because the patient isn’t too exhausted or in too much pain to continue their primary therapy.
2. Supporting Emotional Well-Being
A serious diagnosis affects the mind as much as the body. Palliative teams offer counseling for depression, anxiety, and the existential stress that comes with illness. They also provide a space for families to process the “new normal.”
3. Communication, Clarity, and Goal Alignment
One of the most valuable aspects of palliative care is the “family meeting.” These sessions help patients and their families understand their options. The team acts as a bridge between the various specialists (the cardiologist, the oncologist, the surgeon) to ensure everyone is on the same page regarding the patient’s personal goals and values.
The Financial and Practical Impact
Navigating the healthcare system is notoriously expensive and confusing. Research published in the Journal of the American Medical Association (JAMA) suggests that palliative care can actually reduce overall healthcare costs by preventing unnecessary emergency room visits and hospital readmissions.
Resource Allocation
Addressing the Mental Health Component
My role as an intellectual partner requires me to note a critical intersection here: mental health. In the context of chronic illness, the line between physical pain and psychological distress is thin.
According to the National Institute of Mental Health, patients with chronic physical conditions are at a significantly higher risk for clinical depression. Palliative care acknowledges that treating the body without treating the mind is an incomplete approach. By integrating mental health professionals into the care plan, the team ensures that the “will to live” and the “quality of life” are actively nurtured.
When Is the Ideal Moment to Begin Palliative Care?

The best time to ask for a palliative consultation is now. You don’t need to wait for symptoms to reach a breaking point. Many patients find that starting palliative services early in their diagnosis allows them to build a relationship with the team, making it easier to manage crises later on.
If you find that your illness is making it difficult to perform daily tasks, or if your family is struggling to cope with the demands of caregiving, it is time to speak with your primary physician about a referral.
Palliative Care FAQs: What Patients and Families Ask
1- Does palliative care mean I am dying?
No, it is intended to help you live as well as possible for as long as possible, regardless of the stage of your illness.
2- Will my insurance cover palliative services?
Coverage for palliative care is commonly provided under standard benefits by Medicare, Medicaid, and most private insurers.
3- Can I still see my regular doctor?
Yes, the palliative team works in partnership with your existing doctors to provide an extra layer of support.
4- What care settings offer palliative care support?
It can be provided in a variety of settings, including hospitals, outpatient clinics, or even within your own home.
5- How does it differ from standard medical care?
While standard care focuses on the disease itself, palliative care focuses on the patient’s comfort, symptoms, and overall well-being.
Conclusion and Next Steps for Palliative Care
Palliative care is a transformative approach to medicine that puts the human experience back at the center of the healthcare system. It provides the tools to manage pain, the space to discuss difficult emotions, and the clarity to make informed decisions. By focusing on the quality of everyday life, it empowers patients to live their lives with dignity and comfort, even during the most difficult stages of illness.
If you or a family member is struggling with a complex diagnosis, the next step is to talk with your doctor about your care options. Simply ask: “Could meeting with a palliative care team help reduce symptoms and support a better quality of life?” Taking this step helps ensure that care focuses not only on survival, but on meaningful support throughout the illness.
I’m Salman Khayam, founder and editor of this blog, with 10 years of experience in Travel, Lifestyle, and Culture. I share expert tips on Destinations, Hotels, Food, Fashion, Health, and more to help you explore and elevate your lifestyle.
