When your child is struggling with a persistent stuffy nose or breathing loudly through their mouth, it is easy to assume they have caught another schoolyard cold. However, the culprit is often a pair of small, lumpy tissues located high in the throat known as Adenoidid. While they are a vital part of the immune system during the early years of life, they are also prone to inflammation. Understanding how these tissues function—and what happens when they grow too large—is essential for any parent looking to safeguard their child’s long-term respiratory health and sleep quality.
What Exactly Are Adenoidid and Where Are They Located?
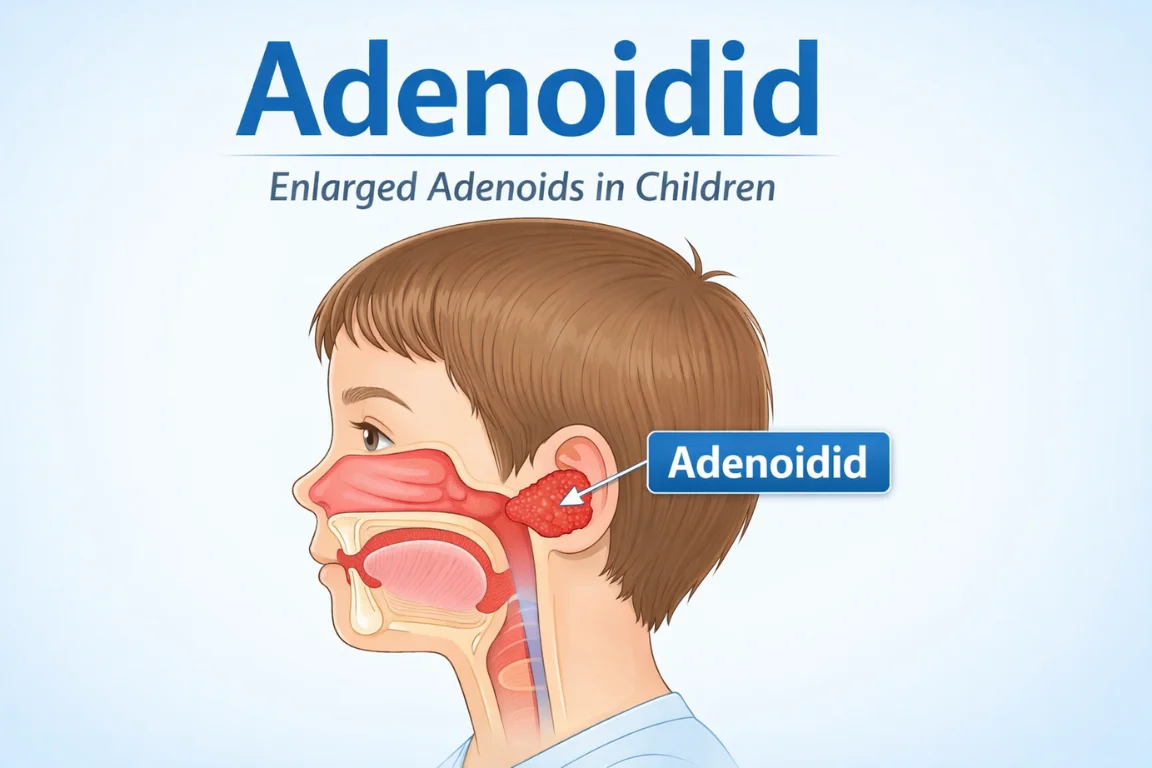
Adenoidid (the plural form of adenoid tissue) are part of the lymphatic system, positioned right behind the nasal cavity and above the roof of the mouth. Functionally, they serve as an early-warning system, monitoring every breath for potential pathogens. Their primary job is to catch bacteria and viruses that a child inhales or swallows. By trapping these pathogens, they help the body build up antibodies, essentially “training” the immune system to recognize future threats.
The Lifecycle of Adenoid Tissue in Children
Unlike your tonsils, which you can see when you open your mouth wide, adenoidid are hidden from view. They are most active and largest in children between the ages of two and six. As a child grows older and their immune system becomes more sophisticated, these tissues naturally begin to shrink. By the time most people reach their teenage years, the adenoidid have usually disappeared or become so small they are no longer functional.
Why Do Adenoidid Become Enlarged or Inflamed?
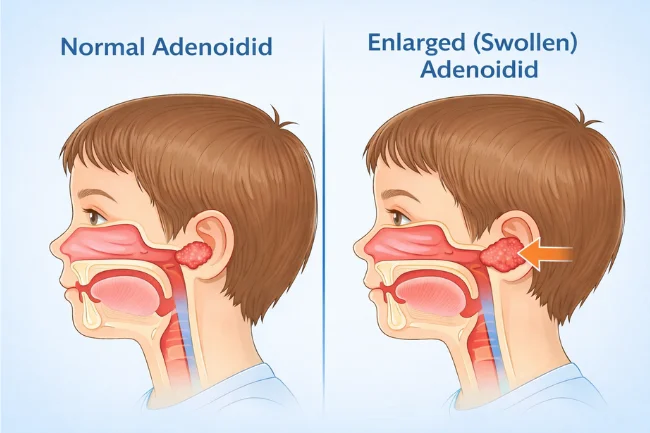
It is perfectly normal for adenoidid to swell temporarily when fighting off an infection. However, in some cases, the swelling persists or becomes chronic. This is often referred to as adenoid hypertrophy.
Common Triggers for Chronic Adenoidid Swelling
Several factors can cause these tissues to remain chronically enlarged:
-
Recurrent Infections: Frequent colds, bouts of bronchitis, or sinus infections keep the immune system in a constant state of “alert,” leading to permanent swelling.
-
Allergies: Chronic exposure to dust mites, pet dander, or pollen can irritate the nasal passages and cause the adenoidid to react.
-
Genetics: Some children are simply born with larger adenoid tissues than others.
-
Environmental Irritants: Secondhand smoke and urban air pollution are significant irritants that can exacerbate tissue growth.
Table 1: Identifying Healthy vs. Enlarged Adenoidid
| Feature | Healthy Adenoidid | Enlarged Adenoidid |
|---|---|---|
| Airway Space | Clear and unobstructed | Narrowed or blocked |
| Breathing Type | Quiet, nasal breathing | Mouth breathing, noisy |
| Speech Quality | Normal resonance | Nasal or “muffled” tone |
| Sleep Pattern | Restful and silent | Snoring or gasping |
Recognizable Symptoms and Red Flags for Parents
Because you cannot see the adenoidid without specialized medical equipment, you have to rely on behavioral and physical symptoms. If your child seems to have a “permanent cold” that never quite clears up, it is time to look closer at their upper airway health.
Breathing Disruptions and Speech Changes
The most obvious sign of enlarged adenoidid is persistent mouth breathing. When the nasal passage is blocked by swollen tissue, the body naturally defaults to the mouth to get air. This can lead to dry lips, a cracked tongue, and a specific “nasal” sound to the voice, as if the child is pinching their nose while speaking.
The Impact of Adenoidid on Sleep and Behavior
Obstructed airways frequently lead to Obstructive Sleep Apnea (OSA). You might notice your child snoring loudly or, more concerningly, experiencing brief pauses in breathing followed by a sharp gasp. This poor sleep quality often manifests during the day as irritability, difficulty concentrating in school, or excessive daytime fatigue.
Ear and Sinus Complications Linked to Adenoidid
The adenoidid sit very close to the Eustachian tubes—the tiny channels that connect the middle ear to the throat. When the tissues swell, they can block these tubes, preventing fluid from draining. This leads to:
-
Chronic Ear Infections: Frequent pain and pressure in the ears.
-
Glue Ear: A buildup of thick fluid that can temporarily impair hearing.
-
Sinusitis: Persistent sinus pressure and yellow or green nasal discharge.
Diagnosis: How Doctors Evaluate Hidden Adenoidid
If you suspect an issue, an Ear, Nose, and Throat (ENT) specialist is the best point of contact. Because the tissue is hidden, they use specific diagnostic tools to get an accurate measurement.
Physical Examination and Nasal Endoscopy
The most common method is a nasal endoscopy. The doctor uses a thin, flexible tube with a small camera to look through the nose and view the adenoidid directly. While it sounds intimidating, it is a quick procedure that provides immediate answers. In some cases, a simple lateral X-ray of the neck can show the size of the airway and the extent of the obstruction.
Management and Medical Treatment Strategies for Adenoidid

Treatment for adenoidid isn’t “one size fits all.” It ranges from watchful waiting to surgical intervention depending on how much the condition interferes with the child’s daily life and development.
Conservative and Medical Management
If the symptoms are mild, doctors often start with non-invasive methods:
-
Nasal Steroid Sprays: These can help reduce inflammation over several weeks.
-
Antihistamines: Useful if allergies are the primary trigger for the swelling.
-
Antibiotics: If a bacterial infection is causing the enlargement, a course of medication may shrink the tissue back to normal size.
Surgical Intervention: The Adenoidectomy Procedure
When medical management fails, or if a child is suffering from severe sleep apnea and hearing loss, an adenoidectomy is often recommended. This is a very common, routine surgical procedure performed under general anesthesia. The tissue is removed through the mouth, so there are no external incisions. Recovery usually takes about one to two weeks, with most children seeing an immediate improvement in their breathing and sleep quality.
Table 2: Adenoidid Treatment Options Overview
| Severity of Obstruction | Recommended Approach | Typical Intervention |
|---|---|---|
| Mild | Observation | Saltwater nasal rinses, monitoring |
| Moderate | Medical | Nasal steroids, allergy management |
| Severe | Surgical | Adenoidectomy (Removal) |
The Role of Nutrition and Home Care in Managing Adenoidid
While diet alone cannot “cure” physically enlarged adenoidid, supporting the immune system is a critical part of management. A body that isn’t constantly fighting off minor infections is less likely to have chronically inflamed tissues.
Supporting the Immune System Through Nutrition
Focus on anti-inflammatory foods. Omega-3 fatty acids found in fish or walnuts can help modulate the body’s inflammatory response. Reducing excessive sugar intake is also beneficial, as high-sugar diets are often linked to suppressed immune function and increased mucus production, which can irritate the adenoidid area.
Improving Environmental Hygiene
Reducing the “load” on the adenoidid is essential. Using a HEPA air purifier in the child’s bedroom can remove dust and pollen that might be aggravating the tissues overnight. Ensuring the home is strictly smoke-free is perhaps the single most important lifestyle change a parent can make to help a child with respiratory issues.
FAQs About Adenoidid
1. Can adenoidid grow back after they have been surgically removed?
While rare, it is possible for adenoidid to regrow if a small amount of tissue is left behind during surgery, especially in very young children. However, this is uncommon and usually doesn’t require a second operation.
2. Is mouth breathing really that harmful for a child?
Yes. Chronic mouth breathing can actually change the development of a child’s facial structure, leading to a narrowed jaw and dental crowding. It also prevents the air from being filtered and humidified by the nose before it reaches the lungs.
3. At what age should I be concerned about my child’s snoring?
It is common for children to snore temporarily when they are congested or fighting off a cold. However, if your child snores more than three nights a week or seems to struggle for breath, you should consult a pediatrician or ENT specialist immediately to check for enlarged adenoidid.
4. Will removing adenoidid weaken my child’s immune system?
According to the American Academy of Otolaryngology, there is no evidence that removing adenoids weakens the immune system. Other lymph nodes and the tonsils take over the protective role immediately.
5. How do I know if it’s allergies or enlarged adenoidid causing the blockage?
Allergies usually come with itchy eyes and sneezing. Enlarged adenoidid cause constant obstruction regardless of the season or environment. A specialist can distinguish between the two through a thorough examination.
Next Steps for Your Family
If your child is showing signs of persistent nasal congestion, restless sleep, or muffled speech, don’t wait for them to “grow out of it.” While adenoidid do shrink naturally over time, the years spent struggling with poor sleep or hearing loss can impact a child’s development and school performance.
Your next step: Keep a sleep diary for one week, noting any snoring or gasping, and bring this data to your pediatrician. Early intervention is the key to ensuring your child breathes easily and stays healthy.
Sources for Further Reading:
-
Mayo Clinic: Adenoiditis and Adenoid Hypertrophy
-
American Academy of Pediatrics (AAP) HealthyChildren.org
-
Cleveland Clinic: Adenoidectomy Recovery and Care
Learn about Holisticke
I’m Salman Khayam, founder and editor of this blog, with 10 years of experience in Travel, Lifestyle, and Culture. I share expert tips on Destinations, Hotels, Food, Fashion, Health, and more to help you explore and elevate your lifestyle.
